[Epistemic status: The claims here are based on my attempt at a thorough reading of peer-reviewed research and Open Philanthropy’s modeling, but I have no formal medical training beyond college level biology and chemistry. I have a pro-harm reduction bias, both as an advocate in my local community and as a recipient of funding from an aligned organization with past ties to the tobacco industry. For more detail, please see the About page.]
Summary: This is the first in a series of posts examining a few of the core claims of tobacco harm reduction advocates from an effective altruist perspective. While experts across a range of views on tobacco harm reduction agree that noncombustible products are at least an order of magnitude less harmful than cigarette smoking, we don’t currently have any rigorous quantification of the risks and benefits of nicotine taken in various noncombustible forms. Supporting the development of better models could be highly impactful. Rough modeling across a wide range of plausible risk levels still supports the tractability of noncombustibles in helping to address the health risks from smoking despite the current lack of clarity.
Introduction
Tobacco harm reduction (THR) advocates argue that reduced risk products such as nicotine pouches, snus, and vapes should be viewed as an integral part of our approach to reducing death and disease from smoking. Having laid out some of their core claims in my previous post, I want to follow up by examining each of them through an effective altruist (EA) lens. The purpose is twofold: to get a better understanding of how well THR-related interventions fit as a cause area given the longstanding interest from EAs in smoking in the developing world, and to gain insight into the community more broadly as an example of “non-EAs who seek to do good.”
The first claim: nicotine isn’t particularly dangerous and its risks are generally overstated due to its historical association with smoking. Perhaps the most-cited THR quote of all time is Michael Russell’s assertion that “people smoke for nicotine but they die from the tar.” The science has advanced considerably since he made that claim in 1976. Advocates continue to argue that “nicotine itself is relatively safe” and that it is “no more harmful to health than caffeine.”
Why does this matter? Even the stauncher skeptics of THR as a policy agree that heated tobacco products (HTPs), vaping, snus, and nicotine pouches are significantly less harmful overall than cigarette smoking. Majorities of not just the general public but of the medical practitioners to whom they look for advice aren’t just unaware of this, but believe the exact opposite. For an EA, doesn’t that in itself strongly suggest importance and neglectedness of THR given the number of smokers in the world is more than a billion and growing, and several million of them die an average of a decade earlier each year?
Maybe so, a skeptic might say, but there’s a big question of tractability: promoting any kind of nicotine or tobacco product as safer runs the risk of more people who wouldn’t have been smokers using it and being harmed by it, potentially wiping out the gains from the current and future smokers who switch. Communicating about their relative safety compared to smoking may also cause people to overestimate their substantial absolute risk to health. It’s all well and good for governments and industry to insist that these are tools meant exclusively for smokers to reduce harm, but it’s reasonable to think nontrivial numbers of non-smokers would start using them if they were more widely viewed as mostly harmless and more extensively promoted. (To say nothing of the “gateway hypothesis” that use of noncombustibles might even cause subsequent smoking - but that’s a story for another post.)
The goal of this post, then, is to examine two questions relevant to EA’s about the claim that nicotine is relatively harmless. Is it true? And to the extent it is, how should that impact our judgment of the tractability of THR interventions?
Translating the claim into DALYs
“Nicotine isn’t particularly dangerous” isn’t specific enough of a claim to say much of any use about, so I’ll tweak it a bit to something that gets to the core of what the advocates say, but allows us a better look from an EA perspective. EAs commonly try to quantify the impacts of problems and proposed solutions to them in terms of disability-adjusted life years (DALYs) gained or lost. The effect of the use of nicotine on a population depends on dosage and method of ingestion. So a reasonable question to ask is “to what extent would the DALYs gained or lost as a result of broader daily use of the most popular noncombustibles affect our estimate of the net effects of promoting them?”
Unfortunately, it’s quite challenging to assign a specific number or even a range of DALYs either for a specific product category or for noncombustibles overall. There are a couple of issues that plague research across product types that are unique to this field:
Lack of randomized, controlled trials: for obvious ethical reasons, there haven’t been any experiments giving nicotine and tobacco products to nonsmokers for extended amounts of time and seeing what happens to them.
Lack of long term information: most of the products are so new that we have at best a decade or two of data on nonsmokers that have used them. Snus is a notable exception here, as it’s been used for hundreds of years in Sweden.
Product heterogeneity: HTPs and e-cigarettes were commercialized very recently, and product development has been rapid, so even someone that has been vaping for 10-15 years has likely used a number of different technologies with potentially different risk profiles. This is even true for snus, as the Gothiatek standard that significantly reduced the concentration of tobacco-specific nitrosamines (TSNAs) and other potentially risky components was implemented gradually across the last few decades.
These problems come in addition to those inherent to evaluating the level of risk of any ingested substance: research on in vitro and animal models is plentiful but the potential risks and benefits they demonstrate often don’t pan out in the real world, and population-level epidemiological work is littered with confounds — maybe even increasingly so, as tobacco use becomes more correlated to demographic attributes with causal impacts on health.
We don’t have rigorous estimates
Most attempts to survey the overall risks of noncombustibles try to answer a slightly different question, and usually focus on one specific product category: does it represent a significantly lower health risk than cigarettes, and are smokers are likely to switch to it?
The Norwegian Institute of Public Health published a thorough report on snus in 2014 and updated it five years later with a couple more studies. The National Academies of Science in the US worked on something similar for vaping. A Cochrane review examined heated tobacco products in 2022. These reviews all provide substantial evidence that each of them are significantly safer than and help people quit smoking, but none of them attempt even an approximate quantification of their overall absolute risk.
A paper on snus from 2004 reports the first attempt I’m aware of to quantify the risk of a noncombustible category. A panel of nine experts was asked by email to answer the question: “Relative to the risk to a lifelong smoker of conventional cigarettes (e.g., Marlboro Red and Newport), what is the relative risk of premature total mortality to a lifelong user of LN-SLT products (e.g., Ariva and Swedish snus)?” The median answer was 9% for ages 35-49 and 5% for ages 50+. Interestingly, the estimates ranged from 0% at the low end to 75% at the upper end, with only two of the panelists rating themselves as “very confident” in their estimates even after three rounds of estimation. One of them also “began with and continued to submit estimates higher than all others” and “provided no comments to justify his/her response, even after panel co-members had criticized the estimates” and was therefore dropped from the final calculation. The paper provides little detail on how each expert arrived at their number.
A more recent and broadly disseminated estimate is the report from the Royal College of Physicians (RCP) in the UK on vaping, cited numerous times by THR advocates and reaffirmed in subsequent evidence reviews: “Although it is not possible to quantify the long-term health risks associated with e-cigarettes precisely, the available data suggest that they are unlikely to exceed 5% of those associated with smoked tobacco products, and may well be substantially lower than this figure.”
While admirably cautious in its phrasing, the report also never elaborates on any details of the modeling that led to the 5% number. Its preceding paragraph cites a publication that “quantified the likely harm to health and society of e-cigarettes at about 5% of the burden caused by tobacco smoking.” This is an article discussing a two-day workshop during which invited experts estimated the harms of various nicotine-containing products by scoring them on a set of criteria proposed by the UK Advisory Council on the Misuse of Drugs — many of which, like how much their use “contributes to damage at an international level” and “decline in the reputation of the community,” are unrelated to health risks that would directly impact DALYs lost from their use. The report also doesn’t explicitly state whether there’s a connection between RCP’s quantification and the exercise the article describes.
It’s tempting to translate the RCP report’s carefully worded claim into the assertion that we can take the DALY loss from smoking, divide it by twenty, and have a reasonable ballpark estimate of the harm from vaping. In fact, the Open Philanthropy shallow investigation on tobacco control did so, probably because there were no other concrete numbers from credible sources. As the THR skeptics at The Lancet point out, though, we should be clear about the flimsiness of the foundation on which this number rests, and understand that the authors of the report themselves give little indication that it was intended to be used in this way.
Critics who refer to the 5% figure from the RCP report as a “myth” often imply our estimate of risk should be higher. I don’t see a compelling reason for that. I’m not aware of any significant evidence that its authors missed or that has come to light since its publication that would give us reason to do so. It continues to be the case that, as one expert put it in 2024, vaping has “not been linked conclusively with any chronic disease.” The authors of the report itself suspect the number is “unlikely” to be larger than 5% and “may well be substantially lower.”
We could use better models
Realizing how sparse the existing work was and not wanting to let the perfect become the enemy of the good-enough, I initially attempted to try to come up with my own bottom-up quantification based on an exhaustive review of specific conditions plausibly caused or worsened by noncombustibles. This turned out to be wildly ambitious, so although I think the work represents a decent start on an overview of the majority of plausible substantial risks and benefits, I’ve moved these to an appendix below.
So is saying “we don’t really know, probably less than 5%” pretty much all a curious non-expert can do until better research comes along? No - I think there at least two important and actionable conclusions given the current state of affairs.
First, the fact that there’s no explicit modeling of risks for a potentially key set of tools for reducing one of the largest causes of human disease and suffering appears to be a great opening for funding from EAs to help make that research happen. Tobacco companies more or less wrote the book on promoting fake science to undermine the work that demonstrated the harms of cigarette smoking. Some of them continue attempted manipulation of the regulatory process for noncombustibles to protect their own market share. At the same time, majorities of both consumers and medical practitioners continue to be mistaken about basic facts in part thanks to deceptive communication about risks from non-governmental organizations. Given the dearth of funders seen by both advocates for and skeptics of THR as fair arbiters in this space, this looks like a unique opportunity.
Second, the fact that we’re missing this piece of the puzzle doesn’t necessarily imply we should be frozen in inaction until it’s put into place. Skeptics often cite the precautionary principle in arguing that until clearer evidence of the extent of harm is established, access should be restricted as much as possible. But while we don’t and will never know everything, EAs can still model under uncertainty, and have done so in this field as well.
Noncombustibles are still a net positive in most plausible scenarios
To elaborate on that second point and come back to the initial motivation for this post: how much does the answer on noncombustible risk impact our assessment of tractability? Does the question of whether EAs should support THR in some form depend significantly on the difference between the plausible best and worst case scenarios?
Open Philanthropy (OP) modeling shows that across a broad range of estimates of noncombustible risk, there’s a good case to be made that the net expected effect of expanding THR is still positive.
As part of their shallow investigation of tobacco control I mentioned earlier, OP included a back of the envelope cost-benefit analysis of the net effect of e-cigarette use in the UK. For lack of better quantification, they used the Public Health England figure of 5% discussed above as the best-guess DALY reduction for vaping compared to smoking — in other words, if the average smoker loses ten years of life due to smoking, they assumed the average vaper would lose six months.
Holding all the other assumptions of the OP model constant and varying the number on vaping health risk lets us draw some basic conclusions. The break even point at which a world with vaping implies fewer DALYs than one without it is around a 25% harm reduction. In other words, any alternative product with at least the net effect on quitting smoking that they estimate vaping has had, and is at least 25% less DALY-reducing, results in a net positive effect. (Interested readers can check this by playing with cells C19 and C34 of the model.)
That’s all well and good, a skeptic might say, but doesn’t a model with increased risks become much more sensitive to the number of nonsmokers that start using nicotine or tobacco? This is also possible to check using OP’s calculation. Assuming an extreme “worst case” scenario of the entire population becoming daily users, the break even point is around 10% harm reduction. In other words, under the assumptions of the OP calculation, THR is a net positive for any product at least an order of magnitude less harmful than cigarettes — even if the entire nonsmoking population became users of that product and none of them would otherwise have become smokers. (You can see for yourself by increasing “total e-cigarette users” (C6) and decreasing “Percent e-cig users ex-smokers” (C12) and “Percent of ecig users who are dual users” (C24) correspondingly.)
There are a couple of issues I see with this interpretation of the modeling that I’ll try to explore in future posts:
The calculation only considers the current population and ignores anyone not born yet. A more thorough model would incorporate calculations about future generations, which would require assumptions not just about how common future use would be, but the degree to which vaping and other noncombustibles would continue to become safer or less safe.
The assumptions around the rate of existing smoking and its reduction are specific to the UK, and would come out differently in different countries - those with higher rates of smoking would see a greater overall benefit from THR, and vice versa for countries with less smoking.
Accepting the conclusions implies EAs shouldn’t oppose efforts to promote THR. It doesn’t necessarily mean that spending resources on promoting it is cost-effective, compared to OP’s 1,000x threshold, to other efforts to reduce smoking-related illness, or to the broader range of cause areas of interest to EAs.
Appendix 1: Risks
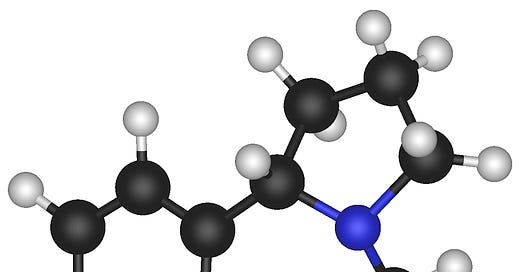
Since the most direct way nicotine affects the human body’s functioning is by binding to the nervous system’s nicotinic acetylcholine receptors, many of its purported risks start with its impact on the brain. These include widely circulated claims that the substance increases the risk of mood disorders, harms brain development, and adversely impacts judgments about risk.
There are a number of plausible risks of health problems unrelated to the brain as well. Most important among these are claims that nicotine use raises the risk of cardiovascular disease, of Type 2 diabetes, and increases the rate of tumor growth.
Mood disorders and cognition
There is plentiful evidence for a correlation between nicotine use and a number of mental health problems. The most well-documented of these associations are with schizophrenia, depression, and anxiety. The important question when assessing the risks is what this correlation implies about the direction of causality. Does a struggle with all or most of these issues result in more people using the substance to manage their symptoms (‘self-medication’) or is there a separate factor, genetic, or otherwise, that makes people more susceptible to certain mental health problems as well as to compulsive patterns of nicotine use? Or are there changes caused directly by the substance that exacerbate these issues?
The link (like most involving smoking) is tricky to study due to the lack of randomized controlled trials. A recent review attempted to address this gap by analyzing research using other methods including co-twin studies and Mendelian randomization. While it examined studies on cigarette smoking in particular rather than nicotine use in general, its results can still be informative — if there’s evidence that smoking doesn’t cause an increased risk of mental illness, that can serve as evidence that nicotine doesn’t, either, as long as there aren’t other factors in smoking causing a commensurate decrease in risk (probably a reasonable assumption).
The review supports the hypothesis that the correlation with depression is due to common liabilities rather than causation: “evidence from co-twin studies indicated that the association with depression was likely completely due to shared genetics. […] [T]here was either no evidence of an effect of smoking or there was evidence for an association in never smokers, suggesting that there is unlikely to be a causal effect of smoking.” Similarly, a longitudinal study of monozygotic twins in Finland showed no effect of smoking on depression.
The causal relationship between anxiety disorders and nicotine use seems a bit less clear. The most extensive review I could find concluded “empirical studies suggest that smoking, and nicotine specifically, can be anxiolytic” but “the parameters and mechanisms through which these effects occur are still poorly understood” and found some evidence from animal studies that “under certain conditions, nicotine can be anxiogenic.” A later but less extensive review similarly concluded that “nicotine may have both anxiolytic and anxiogenic effects at different doses based on the type of anxiety […] and potentially genetic background.”
In the case of schizophrenia, there is an extremely high and well-documented correlation between the two, but not much strong evidence for causality. A large majority (commonly estimated around 80%-90%) of people diagnosed with schizophrenia are daily smokers. There is fairly solid evidence of a variant of a specific gene (CHRNA5) playing a role in hypofrontality, believed to be the cause of many of the symptoms experienced by schizophrenics, and in animal models, nicotine appears to normalize function in the brains of animals with this variant. This provides some support for the self-medication hypothesis. On the other hand, one review examining associations between nicotine and psychosis overall concluded that “self-medication and reverse causation cannot fully explain the association” and that therefore the “jury is out on whether tobacco might be causally related to the risk for psychosis, or whether the association manifests through a shared genetic vulnerability, or is confounded by use of illicit substances or other social factors.” Another recent study, also using Mendelian randomization, concluded “the current evidence that smoking might be a risk factor for schizophrenia is not compelling.”
Development
Even if nicotine is safe for adults, it’s possible that its use affects younger people differently and adversely, both for unborn children whose mothers consume it, and for children and adolescents whose bodies are still developing.
The work I found on neonatal exposure consists mainly of results of animal models describing a number of plausible pathways through which maternal nicotine use could adversely impact prenatal development. A fairly recent review on nicotine replacement therapy (NRT) claims “the main evidence concerning NRT safety and impact on fetal/neonatal brain development is extrapolated from animal studies” and I also couldn’t find any human data on vaping. Two comparisons of mothers prescribed NRT with smokers and nonsmokers looking at risks of stillbirth and congenital anomalies showed no statistically significant risk increase, but since there’s some evidence that NRT in pregnant smokers works no better than placebo for quitting, it’s hard to say how much of it they were actually using.
There is a bit more work on snus. One study found a significant effect on birth weight and preterm delivery - but there was no data and therefore no adjustment possible for alcohol and other psychoactive substance use. Another showed no effect on birth weight for mothers using snus before and in the first eighteen weeks of pregnancy, but so many had quit by then that there wasn’t enough data for later periods. A sibling analysis comparing children born to the same mother during periods of both using and not using snus also found no significant effect on birth weight; the authors conclude “nicotine does not seem to be the main mechanism involved in the association between smoking during pregnancy and birthweight.”
A couple of large population studies on preterm births, stillbirths, oral cleft malformations, and Sudden Infant Death Syndrome found an increased risk for snus users compared to both non-users and those that used but stopped early in the pregnancy. Similarly to the birth weight study, there was no adjustment for alcohol or other psychoactive use in these, but they were able to adjust for a number of other factors including maternal age, BMI, years of education, hypertension, and diabetes.
Nicotine use is also correlated with various risk factors and illicit behaviors in children and teens. One UK study trying to tease out causality, specifically focusing on vaping, found the correlation between having ever vaped at 11 and an increase in various measures of maladjustment and delinquency at 14 was robust to a number of controls including baseline test scores, behavioral measures, and parental education and smoking. This supports the causal hypothesis, although the authors discuss a number of unaddressed potential confounds like the use of other psychoactive substances, as well as the fact that ‘ever use’ is a very rough measure that conflates everyone from one-time experimenters to daily users. Similarly, an analysis of the Population Assessment of Tobacco and Health (PATH) data found an association between ever having vaped and subsequent academic performance among 12 to 15 year olds. A recent scoping review including these and a couple of other studies concluded there is “some evidence that academic achievement may predict future e-cigarette use; less evidence supports the opposite direction.”
There have been a couple of attempts to suss out whether there’s a connection between nicotine use and risk-taking behaviors. One small experimental study found no effect of nicotine on risk taking; two others found it decreased it. All three of these looked at acute effects of nicotine administration in a laboratory setting using the BART task, a well-validated but artificial measure of risk taking behavior. Beside lab-based experimental work, many studies document the correlation between use of nicotine and other behaviors considered risky. A couple of twin studies from Minnesota and Virginia found that genetic predispositions accounted for this correlation rather than nicotine use causing sustained changes in behavior.
Cardiovascular disease
Since smoking is a major risk factor for developing cardiovascular diseases, and nicotine has been shown to have a variety of acute effects on the circulatory system in both animal and human models, it’s natural to ask whether nicotine by itself raises the risk of heart disease, stroke, or other related problems. Most of the population-level research on this topic has been on NRT, snus, and vaping, since none of them are thought to include any other substances that could have an appreciable effect.
A 2024 study used multivariable Mendelian randomization to try to tease out the effects of nicotine from those of smoking on lung cancer, COPD, and heart disease. As some genetic variants are known to be associated with smoking heaviness and others are correlated with speed of nicotine metabolism, this method compares groups based on their genome to tease out the effects of nicotine on smokers separately from other constituents. The authors say the results suggest that “smoking-related outcomes are not due to nicotine exposure but are caused by the other components of tobacco smoke” for all three of the conditions they investigated.
The largest meta-analysis on NRT products I could find concluded that they “do not appear to raise the risk of serious cardiovascular disease events.” However, they did find an elevated occurrence of “less serious events,” mostly tachycardia. Most of the studies reviewed followed NRT users for only up to a year, and restricting the analysis to those of the longest duration made the association “more pronounced and statistically evident.” Since these studies followed only current or former smokers, there may be some risk factors unique to them that don’t apply to the non-smoking population.
Of the three different meta-analyses of the impact of snus I’m aware of, the most recent one found no significant effect on CVD risks. Of the two previous ones, one also found no effect while the second detected an effect on both fatal myocardial infarction and fatal stroke while finding no significant effect on non-fatal events. Some of these studies also include work on other forms of smokeless tobacco used in the US, which show a more consistent effect on CVD. The authors suspect this could be due to other constituents in these products such as tobacco-specific nitrosamines (TSNA’s) whose level is much more strictly regulated in the Swedish products.
In the case of vaping, a Health Canada-sponsored review published in 2025 found a “lack of evidence supporting any association of e-cigarette use with cardiovascular diseases and cardiac dysfunction or remodelling.” This review looked at exposures across a range of time scales (acute, short to medium, and long term).
Diabetes
Smoking has been known for some time to be robustly correlated with the development of Type 2 diabetes (T2D). There is an observable dose-response: more cigarettes smoked increases disease risk. There’s also a plausible biological mechanism: nicotine elevates blood glucose and induces insulin resistance by stimulating the release of catecholamines. Together, these observations lend support to the idea that the relationship is causal, and also applies to noncombustible products.
While I couldn’t find much data on T2D risk in NRT users or vapers, a fairly recent review of the findings on snus use including a number of large longitudinal studies mostly show no significant association between the two. A meta-analysis looking at the data from these and a few others also concluded there was no overall increased risk of T2D in snus users. Interestingly, however, there’s an indication of a dose-response relationship as the heaviest never-smoking consumers did show an elevated risk correlated with their level of use. The Norwegian public health group reached the conclusion that “high consumption,” which the study defined as more than four cans of snus per week, “of Swedish snus among men probably results in a large increase in the risk of type 2 diabetes and metabolic syndrome” while it is “uncertain” whether lower amounts do the same.
Cancer and tumor promotion
A number of health bodies including the International Agency for Research on Cancer, Cancer Research UK, and the American Cancer Society claim plainly that nicotine doesn’t cause cancer. However, there is some evidence suggesting the possibility that health outcomes for people who have cancer are worsened, in particular due to a biologically plausible role of nicotine in tumor growth.
For example, a study of prostate cancer patients in a cohort of Swedish construction workers found a higher risk of mortality (both from the cancer and overall) among those who were regular snus users before the diagnosis. A review of all cancer patients in the same group also found a higher risk of any-cause and cancer-specific death. The authors conclude nicotine is a “conceivable culprit” in the elevated risk while noting a number of limitations of the investigation - notably, risks were adjusted only for BMI, age, and age at diagnosis, and not for any other substance use or lifestyle factors.
The Norwegian public health body’s review on snus concludes that it “probably increases the risk of cancer of the oesophagus and pancreas, and possibly increases the risk of cancer of the stomach and rectum.” This seems to be based mostly on a 2023 review from some of the same authors as the two studies above.
Appendix 2: Benefits
Just as the effects of nicotine have generated numerous hypotheses about conditions it could worsen, a fair number of studies have looked at issues it might help alleviate. The brain and nervous system are again the obvious starting point, but downstream effects provide some plausible candidates for other areas.
Mood disorders and cognition
In the section on risks, I looked at but couldn’t find strong evidence for significant or reliable improvement by nicotine use in any group that’s been studied so far for anxiety, depression, or schizophrenia.
There’s some evidence that smoking is inversely correlated with age of onset of Alzheimer’s disease. As of 2010, a Cochrane review wasn’t able to find any studies on possible causation that met its quality threshold. A pilot study from a few years later showed improvements in several measures of mild cognitive impairment (MCI) after six months of transdermal nicotine treatment. The same group began conducting a larger, placebo-controlled study a few years ago, but haven’t published any results yet.
There’s also been a pretty robust observed negative correlation between smoking and Parkinson’s disease and even some evidence of a causal link. However, the largest placebo-controlled double blind trial conducted to investigate the role of nicotine specifically (using patches) showed no protective effect, at least for patients dosed for one year shortly after initial diagnosis. It’s possible some other component of tobacco smoke causes the effect, or that the timing of the intervention (after Parkinson’s has already been diagnosed) used in this study makes it ineffective, as former smokers also seem to develop the condition at a lower rate.
Body weight and obesity
Smokers tend to gain weight if they quit; they also weigh less on average. There’s a plausible biological mechanism for nicotine’s role involving its effects on energy homeostasis.
The effect of nicotine on body weight is measurable in at least one placebo-controlled trial of patches of former smokers and another of gum. Other studies seem to find no effect on weight gain, though. A recent master’s thesis tested vaping against a control and found an acute effect on subjective appetite but no change in reduced eating.
Gastrointestinal disease
Because smoking seems to be associated with better outcomes for ulcerative colitis, a few trials have looked at whether nicotine delivered via patch or enema could help these patients.
A Cochrane systematic review of a few small RCT’s showed evidence that nicotine administered in this form works better than placebo and about as well as standard medical therapy. There were more patients withdrawing due to adverse events, though, which is presumably why it isn’t actually used therapeutically. A small pilot study also showed an improvement in Crohn’s disease patients - an interesting finding since smoking is known to strongly worsen Crohn’s, which was hypothesized to be related to the effect of nicotine but may be due to other components of smoke.